January 09, 2026
Leading with Purpose: How Molloy Helps Healthcare Leaders Align Mission and Margin
 Healthcare leaders today face an enduring paradox. The responsibility to provide compassionate, high-quality patient care has never been greater, yet hospitals and health systems must operate under mounting financial pressure, workforce shortages, and rapid technological change.
Healthcare leaders today face an enduring paradox. The responsibility to provide compassionate, high-quality patient care has never been greater, yet hospitals and health systems must operate under mounting financial pressure, workforce shortages, and rapid technological change.
Leading with purpose means holding both realities simultaneously: patient care is the mission, and financial sustainability is what keeps that mission alive.
That balance is central to Molloy University’s MBA in Healthcare Administration program, and to how its faculty prepare future healthcare leaders to think and act responsibly.
From the C-Suite to the Classroom
William D. Cundiff, JD, MBA, FACHE, CMPE, CHC, did not follow a traditional academic path into healthcare education. His career spans telecommunications, law, executive leadership, and ownership roles across hospitals, clinics, medical schools, and healthcare organizations in the U.S. and abroad. Before joining Molloy two years ago, he spent decades making high-stakes operational and financial decisions while remaining accountable for patient outcomes.
That owner-operator mindset shapes how he teaches.
“When I speak to students, I tell them patient care is always paramount,” Cundiff says. “It always comes first. But operational and financial decisions directly affect the quality of care. The two are inseparable.”
4 Ways Healthcare Leaders Can Align Mission and Margin
Drawing on real-world leadership experience, Molloy faculty help students confront the decisions healthcare leaders face every day.
1. Treat Financial Stewardship as an Extension of CareHospital expenses continue to outpace revenue growth. In 2024, hospital expenses rose 5.1 percent, significantly exceeding inflation, according to the American Hospital Association.
Purpose-driven leaders view cost control not as compromise, but as stewardship. Financial decisions become ethical decisions when leaders ask how limited resources can best serve patients.
Cundiff often presents practical scenarios: should a facility use a $7 injectable or a $0.36 alternative when efficacy is comparable?
“If we can save money and still provide high-quality care, we can reinvest those savings,” he explains. “That might mean hiring staff, upgrading equipment, improving patient experience, or simply keeping the doors open. Financial discipline enables better care.”
2. Build Retention Strategies Around PurposeBurnout and turnover remain defining challenges. Replacing a single registered nurse costs more than $61,000 on average, according to the 2025 NSI National Health Care Retention & RN Staffing Report. With shortages projected to continue, retention is now a leadership imperative.
“Today’s workforce spans early-career professionals to people nearing retirement,” Cundiff notes. “How you communicate and engage has to adapt. Leaders who connect teams to a shared mission create stability, and that stability improves both care and financial performance.”
Retention, in this sense, is not an HR metric. It’s a reflection of leadership effectiveness.
3. Prepare Clinicians to Lead Beyond the BedsideMany healthcare leaders begin their careers in clinical roles, while others come from operations, finance, or analytics. Leadership requires understanding how clinical outcomes, operational systems, and financial realities intersect.
At Molloy, students learn to link financial data to patient outcomes, apply value-based care principles, and think long-term rather than reactively.
For clinicians, this often means confronting discomfort with finance. Cundiff addresses that directly.
“Nursing and clinical students often panic when they see finance courses,” he says. “We start by saying, ‘We’ve got this.’ These skills are learnable, and essential if you want to lead.”
Students are asked to approach coursework as if they are already practice or service line managers, making decisions that balance care quality, staffing, and sustainability.
4. Communicate Purpose Through Change and InnovationHealthcare organizations are navigating constant change—from staffing models to digital transformation and artificial intelligence. Leaders must guide teams through uncertainty while maintaining trust.
“Engaging staff requires empathy, adaptability, and clarity around purpose,” Cundiff explains. “It requires strong integration between clinical care, operations, and financials.”
Technology adoption follows the same principle. Innovations such as AI must deliver real value. Cundiff often compares AI investment decisions to past management trends: tools matter only if they meaningfully support care delivery and operational effectiveness.
Learning from Leaders Who’ve Done the Work
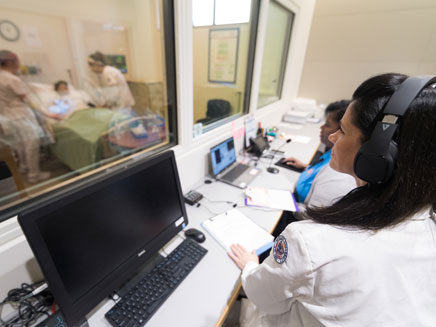
Molloy University’s MBA in Healthcare Administration program serves clinicians preparing for leadership roles, mid-career professionals strengthening their credentials, and early-career students drawn to healthcare administration.
What unites them is access to faculty who have led healthcare organizations through complexity, constraint, and change.
With strong relationships across healthcare systems throughout Long Island, New York City, Westchester, and Connecticut, students benefit from expanded networking, internship, and fellowship opportunities—along with classroom learning grounded in lived experience.
“To keep our patient-first promise, we have to manage wisely and think creatively,” Cundiff tells his students. “That’s how purpose and performance stay aligned.”
Learn more about Molloy University’s MBA in Healthcare Administration.


